Abstract
Introduction
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of NHL ~30% of newly diagnosed lymphoma cases. The International Prognostic Index (IPI) has been the primary clinical tool used to predict outcome for patients with large B-cell lymphomas (LBCL) and used in most clinical trials so far. This model identified five factors to predict DLBCL survival: age >60, elevated serum lactate dehydrogenase (LDH), ECOG performance status ≥2, Ann Arbor stage III or IV, and number of involved extranodal sites ≥2.
This is a single center study aimed to study several clinicopathological characteristics of LBCL including: IPI parameters, double expressor status (DE) and patient's response at end of treatment by Positron emission tomography with 2-deoxy-2-[fluorine-18 ]fluoro- D-glucose integrated with computed tomography (18F-FDG PET/CT) (PET/CT scan). All relevant parameters were correlated to overall survival (OS) and event free survival (EFS). We found an excellent correlation between achievement of post treatment complete metabolic remission (CMR) by PET/CT and both OS and EFS while no statistically significant difference detected regarding OS or PFS among different IPI risk groups or in patients with DE phenotype compared to non-DE.
Patient and Method:
This is a 5- year mixed design study of adults with LBCLs. Baseline demographic, relevant laboratory data including LDH, pathological characteristics: cell origin of lymphoma, KI67 index, relevant immunohistochemical profile, DE status, achievement of CMR at end of treatment were correlated with OS and EFS at 2-years of diagnosis.
Double expressor lymphomas (DELs) are defined by concomitant expression of MYC and BCL2 detected by IHC (cutoffs-40% MYC and 50% BCL2). Genetic double hit lymphomas (by FISH) were excluded.
All patients in our cohort were treated with RCHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) plus Rituximab regimen and evaluated at end of treatment by PET/CT scan using the Deauville five-point scale with scores of 1-3 considered negative and scores 4-5 is positive. All residual lesions exhibiting equal or less intense uptake than the liver were reported as CMR. PET/CT was done six to eight weeks after completion of chemotherapy and 12 weeks after the completion of radiation therapy.
Results:
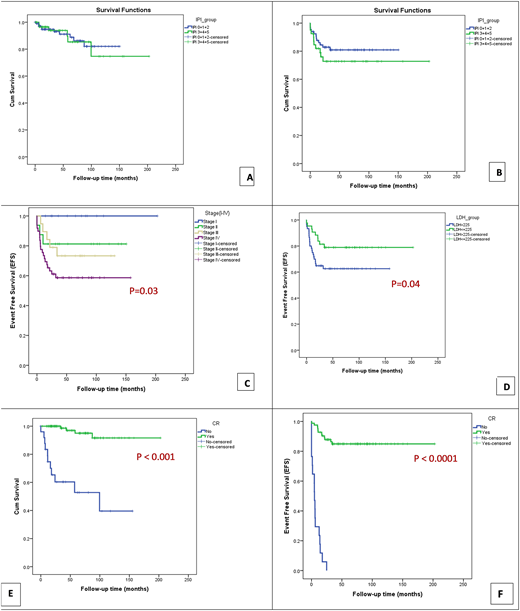
Our cohort was composed of 170 patients diagnosed as large B cell lymphoma, the EFS and OS curves demonstrate the excellent outcome in patients treated with R-CHOP. No statistically significant difference in OS or PFS among different IPI risk groups (1-2 versus 3-5) in our cohort. Disease stage and LDH level had affected EFS with statistically significant differences but not OS. Other individual IPI parameters showed no significant correlation OS or PFS. Although the difference in survival between the two groups (DE and non-DE) are not statistically significant, it was clinically significant with a difference in survival between the two groups of approximately 24 months.
OS and EFS among patients with CMR found to be significantly longer compared to those who did not achieve CMR with a statically significant difference (p:< 0.05). CMR was noted to be higher among patients with favorable IPI (0 to 2) compared to patients with IPI values ranged between 3 - 5, however this difference was statistically insignificant (84.9 % vs 75.5%; P=0.178).
The percentage of post treatment CMR was significantly higher among patients presented without extranodal disease compared to patients with extranodal involvement (94.1 % vs 74.1%; P=0.004). CMR was also significantly higher among patients presented with normal LDH compared to patients with high LDH (91.4 % vs 73.6%; P=0.009).
The percentage of CMR was slightly higher among DE patients compared to non-DE patients , however this difference was statistically insignificant (83.3 % vs 79.6%; P=0.660).
Conclusion
While IPI is the most widely used prognostic predictor in LBCLs, there are limited data regarding the predictive value of post treatment PET/CT scans. We found that achievement of CMR at end of treatment was a very strong predictor of OS and PFS in our cohort compared to standard international prognostic parameters.
To characterize the most important individual IPI parameters affected post treatment CMR and indirectly predicting OS and PFS, we found that extranodal involvement and LDH level were the most significant factors affecting CMR achievement.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal